URETERIC STRICTURE
- Home
- URETERIC STRICTURE
URETERIC STRICTURE - CAUSES, SYMPTOMS, DIAGNOSIS, TREATMENT
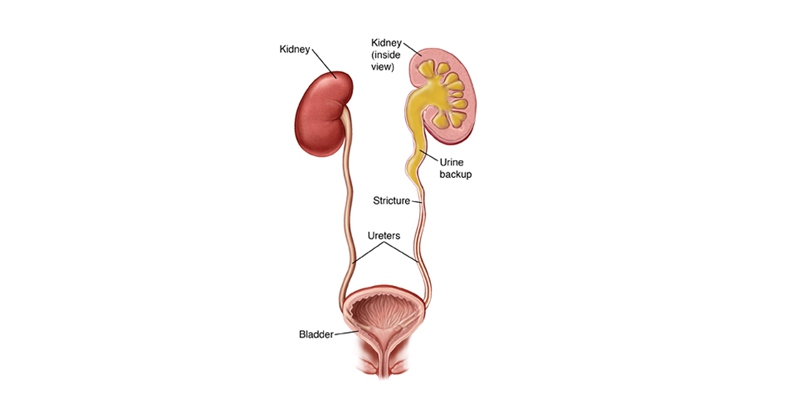
Ureteral stricture is a narrowing of the lumen of the ureter, the duct that carries urine from the kidneys to the bladder, resulting in an obstruction. Ureteral stricture may arise from a variety of causes and is characterized as either anastomotic or nonanastomotic, depending on how they develop. They may be benign or malignant.
Who get it?Any individual undergoing treatment such as an ureteroscopy for kidney, ureteric stone management or urinary diversion is at great risk for developing ureteral stricture.
Ureteric Stricture Causes
Ureteral stricture may be caused by external trauma or may develop after treatment for another condition. Ureteral stricture may be inflammatory due to gonorrhea, tuberculous uretritis, or schistosomiasis, or a rare complication of cancer.
Non-anastomotic ureteral stricture may develop after stone impaction or upper urinary tract endoscopy, as well as following pelvic radiation therapy and a variety of open and laparoscopic surgical procedure or other trauma. Anastomotic ureteral stricture may develop as a result of urinary diversion surgery.
Ureteric Stricture Symptoms
Symptoms of ureteral stricture may include pain, loin lump , flank tenderness, and/or urinary tract infection.
Diagnosis of Ureteric Stricture
It is diagnosed by IVU (Intraveneous Urogram) or retrograde urethrogram to determine the site and degree of stricture.
Ureteric Stricture Treatment
There are a variety of minimally invasive treatments for patients with ureteral strictures. A doctor may perform balloon dilation as a first step in treatment, particularly in patients who have nonanastomotic strictures.
For ureteral strictures that do not respond favorably to dilation alone, endoscopic incision is the procedure of choice for most patients. Endoscopic incision of the stricture can be performed or a laser may be used with a rigid or flexible ureteroscope. A stent may be left in place to keep the ducts open for approximately 6 weeks.
New technique called Holmium Laser Endoureterotomy is now available that may allow long-term relief from ureteral stricture if other techniques are unsuccessful.